We’re Here to Help
Our dedicated team will help you secure approval by providing your insurance company with supporting clinical evidence about your case. We will work with you to complete all the paperwork, explain to your insurance company the reasoning behind your treatment plan, and assist you with the appeal process as needed.
Determining Your Coverage
Proton beam therapy is covered by Medicare, Medicaid, and many private insurance companies. Coverage is determined on a case by case basis depending on your diagnosis, medical history and other factors.
Our Financial Counselor team will work with your primary oncologist to obtain and send all required clinical information to your insurance company to request and obtain authorization prior to scheduling treatment. We will also inform you of any deductibles or out-of-pocket expenses. The New York Proton Center has a financial assistance policy that allows patients to apply for a discount to cover some medically necessary out-of-pocket expenses not covered by insurance.
Our Commitment to Assisting with Appeals
If your insurance carrier determines that your case requires further review, your first request might be denied. This happens often so don’t get discouraged. In fact, it might take several appeals before your submission is approved. We will support you through this process. We can respond directly to insurer questions, write letters of medical necessity, provide supporting documentation, participate in peer-to-peer discussions involving your case and provide comparative treatment plans as requested.
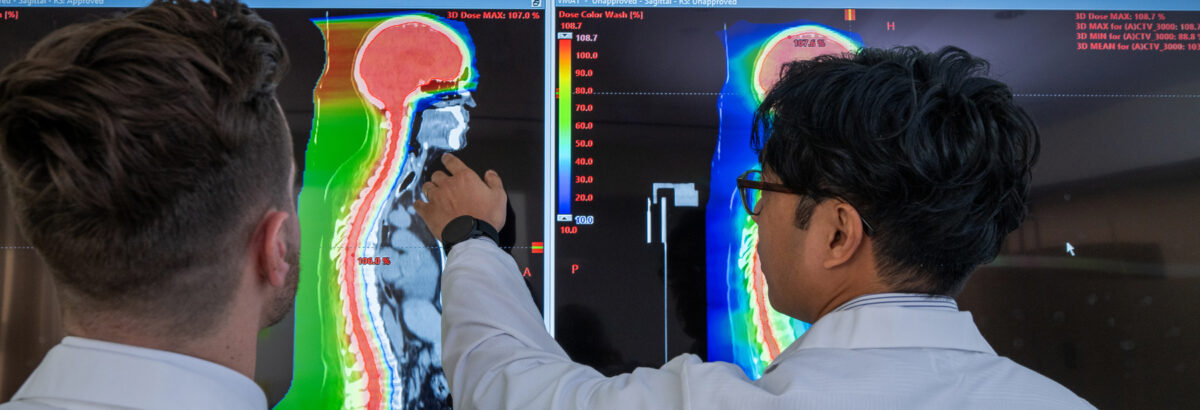
A Proven, Effective Treatment
Clinical data validates proton therapy as an effective cancer treatment that is neither experimental nor investigative. We can share our research validating proton therapy as an effective cancer treatment with your insurance provider.
With You Every Step of the Way
From the moment you contact us, our team will warmly assist you throughout your proton therapy treatment at our center.